Respiratory rate refers to the number of breaths you take in one minute, and understanding what is a normal respiratory rate is crucial for assessing health. For adults, a normal range typically falls between 12 and 20 breaths per minute. In children, this number varies significantly depending on age. For instance, infants may breathe as frequently as 30 to 60 times per minute, while older children average 18 to 30. These variations reflect developmental differences and highlight the need for careful monitoring.
Tracking your respiratory rate can provide early clues about health issues. Studies show that centile charts for respiratory rates help distinguish between what is a normal respiratory rate and abnormal patterns, especially in children. Monitoring this vital sign enables you to detect acute illnesses, assess treatment responses, and maintain overall wellness.
Key Takeaways
- Respiratory rate counts how many breaths you take each minute.
- It shows how healthy your breathing is.
- Normal rates depend on age: adults breathe 12-20 times a minute.
- Babies breathe faster, usually 30-60 times a minute.
- Watching your breathing rate can catch health problems early.
- Things like age, fitness, and feelings can change your breathing rate.
- Checking it often helps you stay aware of changes.
- You can count breaths yourself or use devices to measure them.
- Count for one full minute to get the best results.
- Look out for signs like trouble breathing or feeling confused.
- If these happen, talk to a doctor right away.
- Tracking your breathing can improve your health and manage conditions.
- Knowing your breathing rate helps you stay in control of your health.
What Is Respiratory Rate?
Definition and Role in Health
Respiratory rate measures the number of breaths you take per minute, serving as a fundamental indicator of your respiratory health. This vital sign reflects how efficiently your lungs deliver oxygen to your body and remove carbon dioxide. Normal respiratory rates differ across age groups, with adults typically breathing slower than children. For example, infants may breathe 30–60 times per minute, while adults average 12–20 breaths per minute.
Several factors influence respiratory rate, including physical activity, emotional states, and medical conditions. Fever, dehydration, and infections often increase breathing rates, signaling your body’s effort to meet higher oxygen demands. Conversely, conditions like sleep apnea or certain medications may slow your breathing. Monitoring this metric helps identify potential health issues, such as insufficient oxygen intake or abnormal carbon dioxide levels.
Tip: To better understand what is a normal respiratory rate for your age group, refer to the table below:
| Age | Breaths per minute |
|---|---|
| birth to 1 year | 30–60 |
| 1–3 years | 24–40 |
| 3–6 years | 22–34 |
| 6–12 years | 18–30 |
| 12–18 years | 12–16 |
| over 18 years | 12–20 |
Why It’s a Vital Sign
Respiratory rate is one of the four primary vital signs, alongside temperature, blood pressure, and pulse rate. It plays a crucial role in detecting early signs of health deterioration. Changes in your breathing pattern can indicate serious conditions like sepsis, respiratory failure, or metabolic imbalances. For example, faster breathing may result from anxiety or panic attacks, while slower breathing could signal underlying metabolic issues.
Healthcare professionals often overlook respiratory rate, despite its predictive value. Studies show that abnormal respiratory rates are among the earliest indicators of clinical events, such as low oxygen levels or excess carbon dioxide. Regular monitoring allows you to catch these changes early, enabling timely intervention and improving outcomes.
Note: Respiratory rate is highly sensitive to your physiological state. It reflects how your body responds to stress, illness, or environmental changes, making it an essential tool for maintaining overall wellness.
What Is a Normal Respiratory Rate?
Understanding the normal range of respiratory rate is essential for evaluating your health. This metric varies significantly based on age, activity level, and other factors. Let’s explore what constitutes a normal respiratory rate for different age groups and the factors that influence these ranges.
Normal Respiratory Rate by Age
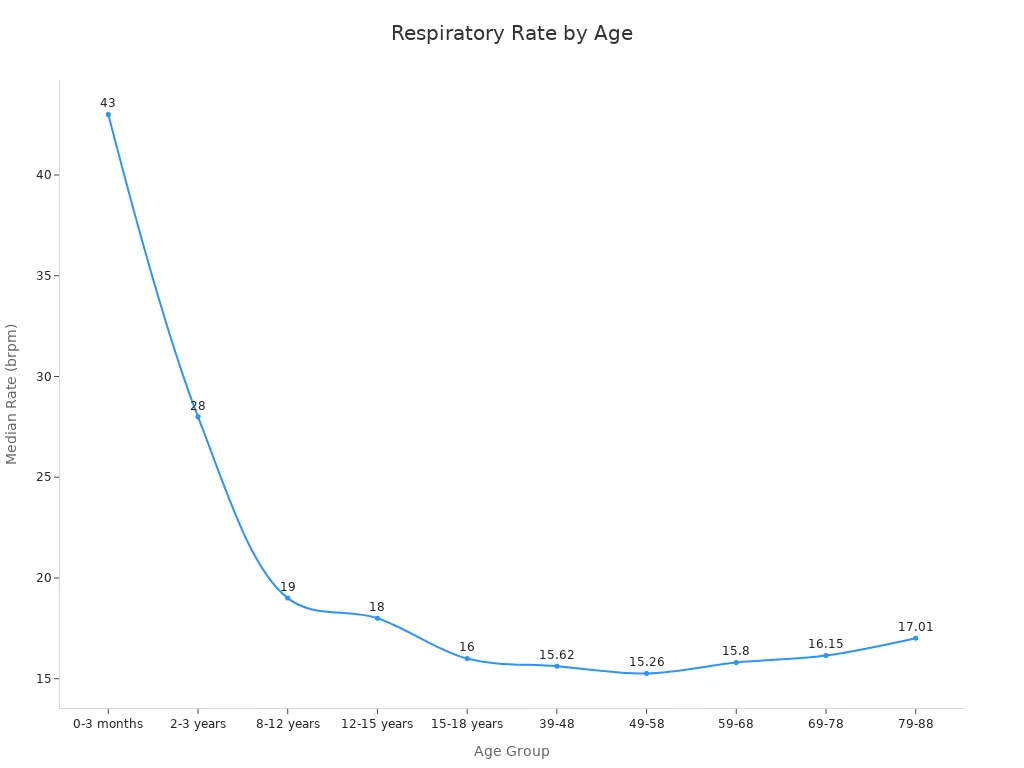
Respiratory Rate in Children
The respiratory rate in children tends to be higher than in adults due to their smaller lung capacity and faster metabolism. For instance, newborns typically breathe 30 to 60 times per minute, while toddlers average 24 to 40 breaths per minute. As children grow, their respiratory rate gradually decreases. By the time they reach adolescence, their breathing rate aligns more closely with that of adults.
| Age Group | Median Respiratory Rate (brpm) |
|---|---|
| 0–3 months | 43 |
| 2–3 years | 28 |
| 8–12 years | 19 |
| 12–15 years | 18 |
This table highlights the typical respiratory rate for children at various developmental stages. Monitoring these rates can help you identify potential health concerns early.
Respiratory Rate in Adults
The normal respiratory rate for adults is generally lower than that of children. Healthy adults typically breathe 12 to 20 times per minute at rest. This range reflects the efficiency of their respiratory systems in meeting oxygen demands. However, age can subtly influence this rate.
| Age Group (Years) | Median Respiratory Rate (brpm) | 5th Percentile (brpm) | 95th Percentile (brpm) |
|---|---|---|---|
| 39–48 | 15.62 | < 12.06 | > 20.06 |
| 49–58 | 15.26 | N/A | N/A |
| 59–68 | 15.80 | N/A | N/A |
| 69–78 | 16.15 | N/A | N/A |
| 79–88 | 17.01 | N/A | N/A |
As shown in the table, the average adult respiratory rate may increase slightly with age. This change often reflects the natural aging process and variations in lung function.
Factors Influencing Normal Ranges
Several factors can affect your normal respiratory rate. These include age, fitness level, emotional state, and environmental conditions. For example, younger individuals tend to have higher respiratory rates due to their developing lungs and higher metabolic demands. In contrast, older adults may experience slight increases in their breathing rate as their lung elasticity decreases.
Physical fitness also plays a role. Athletes and individuals with higher cardiovascular endurance often have lower resting respiratory rates. This efficiency results from their bodies’ ability to deliver oxygen more effectively. Emotional states, such as stress or anxiety, can temporarily elevate your breathing rate. Similarly, high altitudes or polluted environments may cause your respiratory rate to increase as your body compensates for reduced oxygen availability.
How Activity Level Impacts Respiratory Rate
Your activity level significantly influences your respiratory rate. During exercise, your muscles require more oxygen, causing your breathing rate to increase. This response ensures that your body meets the heightened demand for oxygen and eliminates carbon dioxide efficiently.
Interestingly, research shows that lower respiratory rates in men correlate with better physical performance, such as faster reaction times and higher vertical jump heights. However, no significant correlation has been observed in women. These findings suggest that respiratory patterns may vary based on gender and physical fitness levels.
| Finding | Description |
|---|---|
| Lower RR in Men | Associated with better visuomotor reaction times and higher vertical jump heights. |
| No Correlation in Women | No significant correlation between respiratory patterns and physical fitness. |
| Age and Gender Analysis | Results varied by age and gender, indicating a need for further investigation in middle-aged men. |
Understanding how activity impacts your respiratory rate can help you optimize your fitness routine and monitor your overall health.
Importance of Respiratory Rate
Early Detection of Health Issues
Monitoring respiratory rate serves as a critical tool for identifying early signs of health deterioration. Abnormal breathing patterns often precede severe conditions like sepsis, respiratory failure, or cardiac arrest. For instance, studies reveal that respiratory rates exceeding 27 breaths per minute correlate with a 1.72 times higher risk of in-hospital death. This makes respiratory rate a vital indicator of respiratory health and a key predictor of clinical outcomes.
In clinical settings, respiratory rate monitoring has proven invaluable. Research shows that 40% of health deteriorations stem from respiratory issues, and up to 80% of cardiac arrests on general care floors are preventable with timely intervention. However, gaps in monitoring persist, as 75% of patients lack up-to-date vital signs when rapid response teams arrive. Addressing these gaps can significantly improve patient outcomes by enabling earlier detection of critical conditions.
Note: Regularly tracking your respiratory rate can help you recognize subtle changes in your health, allowing for timely medical attention and better management of potential risks.
Monitoring Chronic Conditions
For patients with chronic respiratory or cardiovascular diseases, monitoring respiratory rate is essential. It provides insights into disease progression and helps manage symptoms effectively. For example, individuals with asthma can reduce the frequency of acute episodes by tracking their breathing patterns. Similarly, patients with chronic obstructive pulmonary disease (COPD) can use respiratory rate trends to adjust their treatment plans.
Historical data underscores the importance of respiratory rate as a vital sign. Since the 19th century, it has been recognized as a more reliable predictor of severe complications than heart rate or blood pressure. Modern studies confirm this, showing that consistent monitoring decreases emergency visits and improves overall disease management.
| Benefit | Description |
|---|---|
| Increased awareness of disease status | Patients and providers can track lung function better. |
| Decreased asthma episodes | Monitoring helps in managing and reducing episodes. |
| Decreased acute care visits | Early detection leads to fewer emergency visits. |
| Decreased missed school days | Improved management allows for better attendance. |
By incorporating respiratory rate monitoring into your routine, you can enhance your quality of life and reduce the burden of chronic illnesses.
Connection to Overall Wellness
Your respiratory rate is more than just a number; it reflects your overall well-being. A slower, steady breathing pattern often indicates better physical and mental health. Studies show that individuals with slower respiratory rates report higher levels of well-being after wellness training. This suggests that respiratory rate can serve as a biomarker for overall health.
Statistical analyses further highlight its predictive power. Univariate analysis identifies respiratory rate as the best predictor of clinical deterioration, with an area under the curve (AUC) of 0.70. Standard deviation analysis improves this accuracy to 0.71, emphasizing the importance of monitoring respiratory rate as part of a comprehensive wellness strategy.
| Analysis Type | Findings |
|---|---|
| Univariate Analysis | Respiratory rate was the best predictor of clinical deterioration (AUC 0.70). |
| Standard Deviation | More accurate than current value (AUC 0.71). |
Incorporating respiratory rate tracking into your health routine can help you maintain balance and detect potential issues before they escalate. Whether you are managing a chronic condition or striving for optimal wellness, this vital sign offers valuable insights into your health journey.
How to Measure Respiratory Rate Accurately

Manual Measurement Techniques
Counting Breaths Per Minute
Manually counting breaths per minute remains a widely used method for measuring respiratory rate. This technique involves observing the rise and fall of the chest or abdomen to count the number of breaths within a specific time frame. Studies suggest that counting thorax excursions for 30 seconds and doubling the result provides a reliable estimate. However, counting for shorter durations, such as 15 seconds and multiplying by four, can introduce significant errors.
In clinical settings, visual counting is the standard approach, but it has limitations. For example, it is prone to inaccuracies and is not practical for continuous monitoring, such as overnight recordings. Despite these challenges, manual counting remains a valuable tool when performed correctly.
Tips for Accuracy
To ensure accurate manual measurements, follow these tips:
- Observe the patient in a relaxed state, as stress or movement can alter the respiratory rate.
- Count breaths for a full 60 seconds whenever possible. This minimizes errors compared to shorter counting intervals.
- Avoid alerting the patient to the measurement process, as this may cause them to alter their breathing pattern.
- Use a timer or stopwatch to maintain consistency during the counting process.
Tip: Practice this technique regularly to improve your accuracy and confidence in manual respiratory rate measurement.
Technological Tools for Measurement
Wearable Devices like Circul Ring
Wearable devices have revolutionized how respiratory rates are monitored. Devices like the Circul Ring use advanced sensors to measure breaths per minute continuously and accurately. These tools are particularly useful for overnight monitoring or tracking respiratory patterns over extended periods.

Studies comparing wearable devices to manual counting have shown promising results. For instance, one study found that a wearable optical method demonstrated good agreement with manual counts, with a mean bias of just 0.05 breaths per minute. This highlights the potential of wearable technology to provide reliable and convenient respiratory rate measurements.
Smartphone Apps and Other Tools
Smartphone apps and other digital tools offer another convenient way to measure respiratory rate. Many apps use the phone's camera or microphone to detect breathing patterns and calculate breaths per minute. While these tools are not as accurate as wearable devices, they provide a quick and accessible option for casual monitoring.
Emerging technologies, such as contactless monitoring systems, are also gaining traction. For example, radar-based modules have been tested against gold-standard methods in emergency settings, showing potential for non-invasive respiratory rate monitoring.
| Study Title | Methodology | Findings |
|---|---|---|
| Wearable platform with optical-based approach | Compared wearable optical method to manual counts | Mean bias of 0.05 bpm |
| Automated vs. manual respiratory rate | Compared manual and automated systems | Significant discrepancies in manual documentation |
| Contactless radar module | Validated radar module against gold-standard methods | Promising results for non-invasive monitoring |
Common Errors to Avoid
Accurate respiratory rate measurement requires attention to detail. Common errors include:
- Underestimating mouth pressure swings during respiratory efforts.
- Failing to establish a stable end-expiratory lung volume during relaxed breathing.
- Allowing leaks at the mouthpiece or nose clip during gas dilution techniques.
- Losing the lip seal at the mouthpiece during closed-shutter panting maneuvers.
- Incorrectly pacing the patient's tidal breathing before shutter closure, leading to dynamic hyperinflation.
Avoiding these mistakes ensures more reliable measurements and better health monitoring outcomes.
Note: Whether you use manual or technological methods, understanding the potential pitfalls can help you achieve accurate and consistent results.
Factors That Affect Respiratory Rate
Age and Developmental Stage
Your age and developmental stage significantly influence your respiratory rate. Infants and young children breathe faster than adults due to their smaller lung capacity and higher metabolic demands. For example, newborns typically have a median respiratory rate of 44 breaths per minute, while two-year-olds average 26 breaths per minute. As you grow older, your respiratory rate decreases and stabilizes during adulthood.
| Age Group | Median Respiratory Rate (breaths/min) |
|---|---|
| At Birth | 44 |
| At 2 Years | 26 |
This gradual change reflects the development of your lungs and respiratory system. However, aging can also lead to subtle increases in respiratory rate due to reduced lung elasticity and efficiency. Understanding how your age impacts your breathing can help you identify deviations from normal patterns and address potential health concerns early.
Physical Activity and Fitness Level
Your physical activity and fitness level play a crucial role in shaping your respiratory patterns. Regular exercise strengthens your respiratory muscles and improves lung capacity, allowing you to breathe more efficiently. Elite athletes, for instance, often exhibit higher spirometric lung volumes compared to sedentary individuals. These adaptations result from consistent training and enhanced cardiorespiratory fitness.
Interestingly, while respiratory rate can influence gas exchange variables, it does not directly correlate with physical fitness levels like VO2max or endurance performance. This means that although your fitness level impacts your respiratory function, it may not always align with your respiratory rate patterns. Nonetheless, maintaining an active lifestyle supports overall respiratory health and helps your body adapt to varying oxygen demands during physical exertion.
Emotional and Psychological States
Your emotional and psychological state can cause noticeable changes in your respiratory rate. Stress, anxiety, and other negative emotions often lead to rapid, shallow breathing. This response, known as respiratory sinus arrhythmia, reflects how your heart rate and breathing synchronize during emotional arousal. For example, anxiety can shorten your resting expiratory time and increase your minute ventilation, affecting your blood carbon dioxide levels.
| Study Title | Findings |
|---|---|
| Respiration rate during a stress task moderates neuroticism and perceived stress in older adults | Emotional states, particularly anxiety, can lead to increased respiratory rate. |
| The human ventilatory response to stress: rate or depth? | Anxiety shortens resting expiratory time. |
| Respiratory Rhythm, Autonomic Modulation, and the Spectrum of Emotions | Negative emotions like fear and anxiety result in rapid, shallow breathing. |
| Anxiety and Respiration | Increased anxiety leads to higher minute ventilation. |
By managing stress and practicing relaxation techniques, you can regulate your breathing and maintain a healthy respiratory rate. Activities like deep breathing exercises or mindfulness meditation can help you counteract the effects of stress on your respiratory system.
Medical Conditions and Medications
Certain medical conditions and medications can significantly alter your respiratory rate. These changes often reflect how your body responds to underlying health challenges or external substances. Understanding these influences can help you identify potential risks and take proactive steps to manage your respiratory health.
Several medical conditions directly impact your ability to regulate breathing. These include:
- Stroke: It can disrupt the brain's control over respiratory functions.
- Muscular dystrophy: This condition weakens the muscles required for effective breathing.
- Nerve or spinal cord injuries: Damage to these areas can impair the signals that control your respiratory muscles.
- Multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS): Both conditions affect the nervous system, leading to breathing difficulties.
- Hypothyroidism: This condition slows your metabolism, which can reduce your respiratory drive.
- Anatomical abnormalities: Issues like scoliosis or flail chest can restrict lung expansion, making breathing less efficient.
Medications also play a critical role in altering respiratory patterns. Some drugs, particularly those affecting the central nervous system, can cause respiratory depression. Examples include:
- Opioids: Medications like fentanyl, oxycodone, and codeine slow your breathing and reduce its effectiveness.
- Benzodiazepines: Drugs such as midazolam and diazepam (Valium) can suppress your respiratory drive.
- Polypharmacy: Using multiple CNS depressants simultaneously increases the risk of respiratory complications.
Other factors, such as age (55+), obesity, smoking, and a compromised immune system, can amplify the effects of these medications. If you take any of these drugs or have a condition that affects your breathing, regular monitoring of your respiratory rate is essential.
Environmental Influences
Your environment plays a significant role in shaping your respiratory rate. Factors like air quality, temperature, and even nutritional status can cause noticeable changes in your breathing patterns. A study conducted in rural Gambia highlights this connection. Researchers tracked respiratory rates in 830 children aged 6 months to 14 years, recording over 67,000 measurements. They found that ambient temperature, stunting, and the time of day were significant predictors of respiratory rate. This demonstrates how environmental conditions can directly influence your breathing.
Polluted air, for instance, forces your lungs to work harder to filter out harmful particles, leading to an increased respiratory rate. High altitudes, where oxygen levels are lower, can also cause faster breathing as your body compensates for reduced oxygen availability. Similarly, extreme temperatures—whether hot or cold—can stress your respiratory system, prompting changes in your breathing pattern.
By being mindful of these environmental factors, you can take steps to protect your respiratory health. For example, using air purifiers, staying hydrated, and avoiding strenuous activities during extreme weather can help you maintain a normal respiratory rate.
Abnormal Respiratory Rates: Causes and When to Seek Help

Tachypnea (Fast Breathing)
Causes of Tachypnea
Tachypnea refers to an increased respiratory rate, defined as more than 20 breaths per minute in adults. This condition often arises from various physiological and pathological factors. Common causes include:
- Fever or infection: Your body increases its respiratory rate to meet higher oxygen demands.
- Anxiety or panic attacks: Emotional stress can trigger rapid, shallow breathing.
- Respiratory conditions: Asthma, pneumonia, or chronic obstructive pulmonary disease (COPD) frequently lead to tachypnea.
- Cardiac issues: Heart failure or pulmonary embolism may cause your breathing to accelerate as your body struggles to maintain oxygen levels.
The balance between central and peripheral chemoreceptors, along with airway receptors, plays a critical role in regulating your respiratory rate. These sensors relay information to your central nervous system, which adjusts your breathing to maintain homeostasis. Disruptions in this system can result in abnormal respiratory patterns, including tachypnea.
When It’s a Concern
Tachypnea becomes a concern when it persists or occurs alongside other symptoms, such as chest pain, confusion, or bluish skin. These signs may indicate severe conditions like respiratory failure or sepsis. If your respiratory rate exceeds 27 breaths per minute, it significantly increases the risk of in-hospital complications. Seek immediate medical attention if you notice these warning signs.
Bradypnea (Slow Breathing)
Causes of Bradypnea
Bradypnea, characterized by a decreased respiratory rate, occurs when adults breathe fewer than 12 times per minute. This condition often results from:
- Neurological disorders: Stroke or traumatic brain injuries can impair the brain's ability to regulate breathing.
- Medications: Opioids and sedatives frequently suppress your respiratory drive.
- Metabolic imbalances: Conditions like hypothyroidism slow your metabolism, leading to reduced breathing rates.
In children, the benchmarks for bradypnea differ due to their naturally higher respiratory rates. For instance, a study of postoperative patients aged 60 and above revealed that 78% experienced at least one bradypneic event, with a median duration of 1.4 minutes. These findings highlight the importance of age-specific thresholds when evaluating respiratory patterns.
When It’s a Concern
Bradypnea warrants concern when it leads to symptoms like dizziness, fatigue, or loss of consciousness. Prolonged episodes can result in insufficient oxygen delivery to your organs, causing severe complications. If you experience repeated or extended bradypneic events, consult a healthcare provider promptly.
Other Breathing Irregularities
Breathing irregularities encompass a range of patterns beyond tachypnea and bradypnea. Conditions like hyperventilation syndrome (HVS) and dysfunctional breathing (DB) are prevalent in specific populations. For example, HVS affects 6–10% of the general population but rises to 29% among asthmatics. A study involving 209 patients with unexplained exertional dyspnea found that over half exhibited moderate-to-severe DB, with a prediction accuracy of 78% for DB assessment.
| Study Title | Methodology | Participants | Results |
|---|---|---|---|
| Quantification of breathing irregularity for the diagnosis of dysfunctional breathing | Cross-sectional, retrospective, real-world study | 209 patients with unexplained exertional dyspnea | More than half of the patients affected by moderate-to-severe DB, prediction accuracy of 78% for DB assessment |
Accurate diagnosis of these irregularities remains challenging due to the lack of standardized criteria. However, recognizing patterns like rapid, shallow breathing or erratic respiratory rhythms can help you identify potential issues. If you suspect a breathing irregularity, seek professional evaluation to determine the underlying cause and appropriate treatment.
Warning Signs and Medical Attention
Symptoms to Watch For
Changes in your respiratory rate can signal underlying health issues that require immediate attention. Recognizing these warning signs early can prevent complications and improve outcomes. A sustained respiratory rate exceeding 20 breaths per minute often indicates that your body is under stress. If this rate rises above 24 breaths per minute, it may serve as a critical warning of a serious adverse event within the next 24 hours.
Several symptoms accompany abnormal respiratory rates, helping you identify when medical intervention is necessary:
- Persistent shortness of breath or difficulty breathing.
- Rapid breathing that does not subside after rest.
- Chest pain or tightness during breathing.
- Bluish discoloration of the lips, face, or fingertips, indicating low oxygen levels.
- Confusion, dizziness, or fainting episodes.
Monitoring your respiratory rate can also reveal early signs of severe conditions like sepsis, organ failure, or cardiac arrest. These symptoms often develop subtly, making regular observation crucial for timely detection.
Alert: If you notice any of these symptoms, consult a healthcare provider immediately. Delaying medical attention can lead to life-threatening complications.
Importance of Timely Intervention
Timely intervention plays a pivotal role in managing respiratory rate abnormalities. When your breathing pattern changes, it reflects how your body responds to stress, illness, or environmental factors. Addressing these changes promptly can prevent the progression of severe conditions.
For example, a respiratory rate exceeding 24 breaths per minute often precedes critical events like respiratory failure or cardiac arrest. Early medical evaluation allows healthcare providers to identify the root cause and initiate appropriate treatment. This proactive approach reduces the risk of complications and improves recovery outcomes.
Ignoring abnormal respiratory rates can have dire consequences. Persistent rapid breathing may lead to oxygen deprivation, affecting vital organs like the brain and heart. Conversely, slow breathing can result in carbon dioxide buildup, causing confusion and fatigue. Both scenarios demand immediate attention to avoid irreversible damage.
Tip: Regularly monitor your respiratory rate, especially if you have chronic conditions or are recovering from illness. Early detection empowers you to take control of your health and seek timely care.
Understanding and monitoring your respiratory rate is essential for maintaining good health. This vital sign provides critical insights into your body's oxygenation and overall wellness. Regular tracking helps you detect early signs of illness and manage chronic conditions effectively.
| Vital Sign | Normal Range | Significance |
|---|---|---|
| Respiratory Rate | 12 - 20 breaths/min | Affects overall oxygenation and health |
Using tools like the Circul Ring simplifies this process. These devices offer accurate and convenient measurements, empowering you to take control of your respiratory health. By prioritizing this key indicator, you can enhance your well-being and stay proactive about your health.
FAQ
What is the best time to measure respiratory rate?
Measure your respiratory rate when you are at rest and relaxed. Avoid measuring after physical activity or emotional stress, as these can temporarily elevate your breathing rate.
How can I tell if my respiratory rate is abnormal?
Compare your respiratory rate to the normal ranges for your age group. Persistent rates above or below the typical range, especially with symptoms like shortness of breath, may indicate a problem.
Can stress affect my respiratory rate?
Yes, stress often increases your respiratory rate. Emotional states like anxiety or fear can cause rapid, shallow breathing. Practicing relaxation techniques can help regulate your breathing.
Are wearable devices accurate for measuring respiratory rate?
Wearable devices like the Circul Ring provide reliable respiratory rate measurements. They use advanced sensors to track your breathing continuously, making them a convenient option for monitoring.
How does altitude impact respiratory rate?
At higher altitudes, your respiratory rate increases to compensate for reduced oxygen levels. This adjustment helps your body maintain adequate oxygenation in low-oxygen environments.
Should I measure respiratory rate in children differently?
Yes, children have higher respiratory rates than adults. Observe their chest or abdomen movements for a full minute to ensure accuracy, as their breathing can be irregular.
Can medications influence respiratory rate?
Certain medications, such as opioids or sedatives, can slow your respiratory rate. Others, like stimulants, may increase it. Always monitor your breathing if you take medications that affect the central nervous system.
When should I seek medical attention for abnormal respiratory rates?
Seek immediate medical help if you experience persistent abnormal respiratory rates with symptoms like chest pain, confusion, or bluish skin. These signs may indicate a serious condition requiring urgent care.






